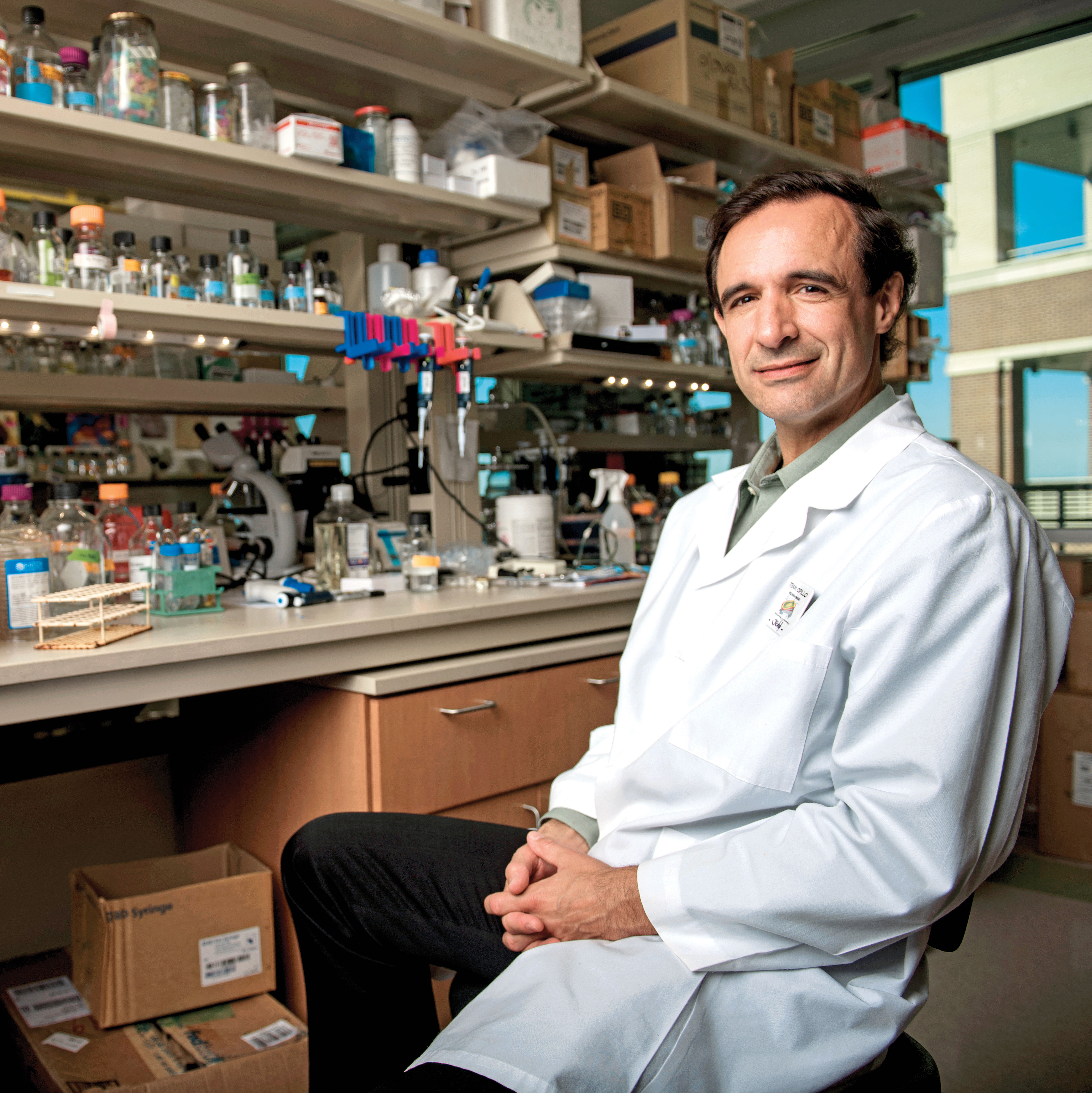
Two "Average Joes" Helping Houston's At-Risk Communities

Dr. Joseph Gathe is helping fight Covid-19 in Acres Homes.
Image: Anthony Rathbun
DR. JOSEPH GATHE WAKES UP AT 4 A.M. every morning and heads to the 117-bed United Memorial Medical Center in Acres Homes. There he changes into layers of protection—scrub suit, hazmat suit, face masks, and a face shield that fogs his glasses, makes his hearing terrible, and renders his stethoscope obsolete. A lanyard with his photo dangles around his neck, so patients will know there’s actually a human being underneath the gear when he makes his rounds at the Covid-19 unit he co-directs with colleague Dr. Joseph Varon. Friends call them “The Average Joes.”
“I don’t know if you’ve ever been in a PPE outfit,” says Gathe, who trained as an infectious disease expert at Baylor during the HIV epidemic before going on to oversee an entire floor of HIV patients at Park Plaza Hospital in the Texas Medical Center. “But when you walk into a patient’s room, you look like you’ve walked out of an Andromeda Strain movie.”
The duo have spent every day since March “bringing people back from the brink of death,” as Varon described it to the Los Angeles Times in July, but they’ve also found time to launch the Cure Covid Consortium, a nonprofit bringing free testing and other resources to Houston communities disproportionately affected by the virus, a disparity they’ve seen play out before them.
“If you look at our unit at any point in time, I’d say 80 to 85 percent of the patients coming in are communities of color, primarily African Americans and Hispanics,” says Gathe. About 60 percent are also uninsured. It’s a concern to those on the front lines, he says, especially as America has failed to enact a cohesive response to the virus and failed to institute widespread testing. “The response in our country is patchwork. Nobody is doing the same thing. You’re not getting a consistent message,” he explains. “And what’s happening in the communities, people see this and just tune out.”
The UMMC Covid-19 unit itself sprung from a testing site. In March UMMC partnered with Sheila Jackson Lee to launch one of the first public, drive-through testing sites in Houston, which immediately resulted in hours-long wait times and hundreds of cars in line.
“People were getting sick in their cars waiting to get tested,”says Gathe. The hospital cordoned off the unit in March, opening with 20 beds to treat such patients.
Yet by April Texas was still conducting a mere 332 tests per every 100,000 residents, and faced with a growing number of inpatients and outpatients—Gathe also treats folks via Zoom every day—he found himself brainstorming with his wife, Deanna, one night about what they could do to help. “We were saying this is a lot like the HIV epidemic,” he recalls. “How are we going to handle this?” They decided to get out into the community and tackle the problem head-on.
Funded by a $1 million grant from the Start Small and BeyGOOD foundations—“We got a call from Tina Knowles, Beyoncé’s mom, and she’s been very helpful,” says Gathe—the Cure Covid Consortium has now tested more than 1,000 Houstonians and anticipates testing thousands more before the end of the year.
Of course, folks who arrive at St. John’s Church or Jack Yates High School will still face some challenges that have plagued Covid-19 testing from the get-go—they must register online, wait in line, get that swab up the nose, and endure the lag time to get results back from overwhelmed laboratories in Texas—at press time in mid-August, an agonizing 7 to 10 days. But Gathe and his team have been able to streamline and improve the testing process in ways that are imperative for at-risk communities.
Registrants don’t even need an ID to get a test, just a phone number for the consortium to contact them afterward to discuss their results. Plus, a team of contact tracers, volunteers from partnering outreach group Bread for Life, helps get in touch with others who could’ve been exposed. Their assistance is vital, not just because contact tracing is lacking in Houston but also because household sizes have increased over the past decade for the first time in 160 years, according to U.S. Census data released last October. An estimated 64 million Americans live in multigenerational homes, a number that’s likely grown since 2016 (the most recent Pew Research Center study available), especially as the pandemic’s economic toll sends folks looking for cheaper living arrangements. “How many grandparents live with their sons and daughters at the house to help take care of them and the grandkids?” asks Gathe. “We need to know that.”
And for those who test Covid-positive and have no insurance, he says, “our contact tracers and sister organizations will be able to put you in a position that you’ll be able to get a health care professional, get access to medication, and even get into a hospital to have treatment and care.”
The sites also serve as places to dispel misinformation about the virus, so Gathe is able to share what doctors and medical experts know and what they don’t know. He’s made a point of stressing key information to those coming in to be tested, namely that a negative test result might not mean you’re really negative. That multiple tests might be necessary. That 15 to 20 percent of people coming to get a test are now testing positive, depending on the neighborhood. And, he notes, “I can’t predict who’s going to get sick or not.”
Gathe watched his own personal trainer—“an ex-NFL tight end, age 40, one of the most healthy people on planet Earth”’—almost die in March, though the man’s wife and kids never contracted the disease. He cheered as a 90-year-old woman with metastasized pancreatic cancer walked out of his unit with a sign that read, Covid ain’t got nothing on me. But by July his unit had grown to 80 beds with 72 additional overflow beds available in the Texas Medical Center, and he was seeing a high percentage of people coming into UMMC between the ages of 20 and 50 with no co-morbid conditions at all. He and Varon have been working almost constantly for months, but Gathe shrugs that off, saying that the main thing is to get the message out, to save as many people as possible. And his core message is so simple.
“The one thing, out of everything on planet Earth, that mitigates this disease process is wearing a mask,” he says. “To decrease the spread of the virus, in all communities—but especially the African American community, where we have these particular issues, where people tend to be closer together—that’s the one thing that changes everything.”