We're Living in Traumatic Times Thanks to Coronavirus, So Don’t Be So Hard on Yourself

Image: Courtesy Shutterstock/jiris
If there’s one word to describe the general mood these days, tense might be an apt choice. We've been stuck inside for weeks on end as a pandemic far greater than we could have imagined ravages our world, taxing our hospital systems, and wreaks havoc our global economy. On top of that, there's no clear end in sight. "We handle things much better when we know that there's an expectation of relief and right now, we don't know," says Dr. Ben Weinstein, chair of psychiatry at Houston Methodist. " No one knows.”
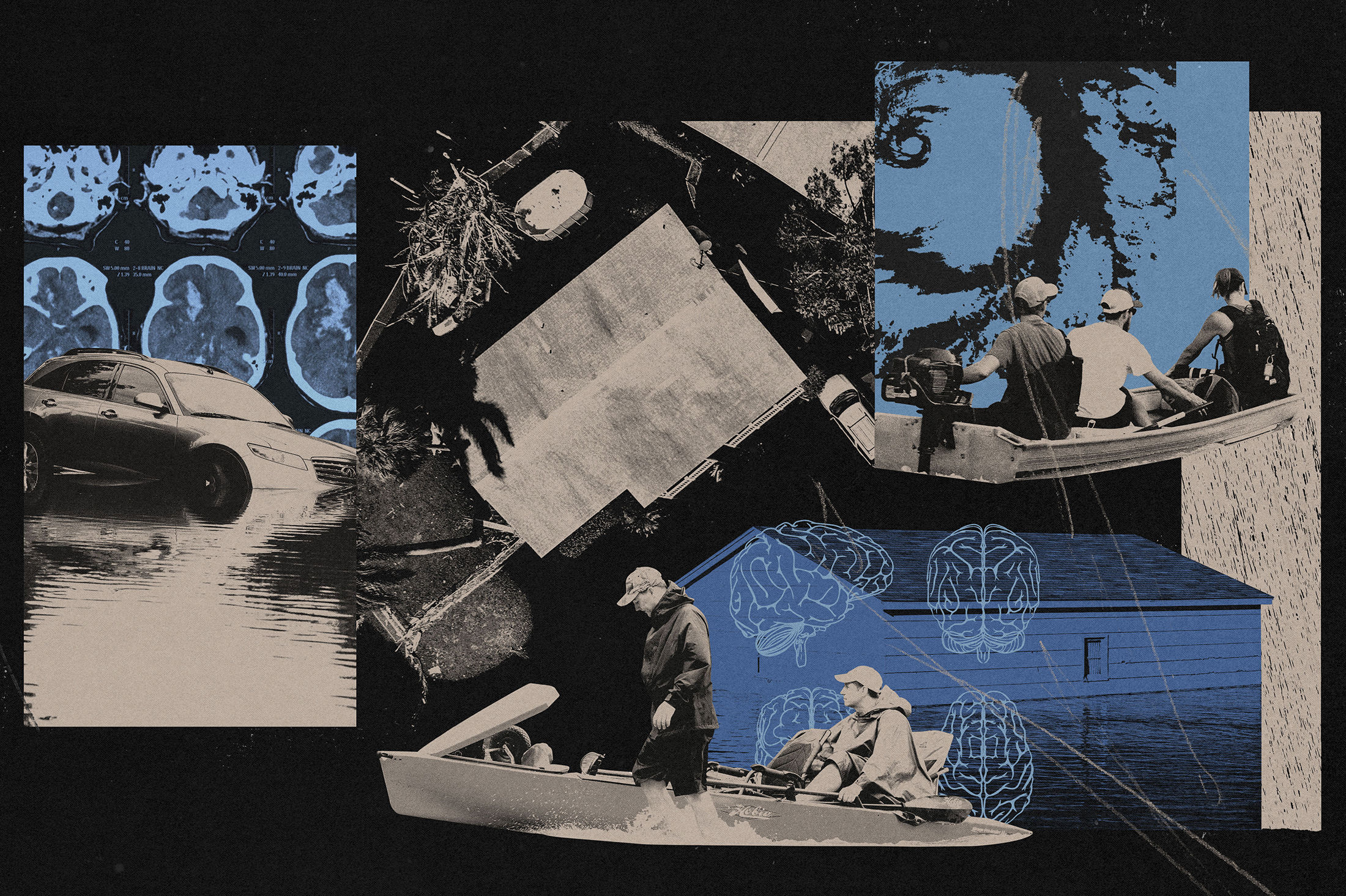
Because of these factors, some in the mental health community are pointing to a different t-letter word to describe our current experience. “We are in a traumatic situation,” says Neal Sarahan, executive director of NAMI Greater Houston. “We come to COVID-19 with a whole set of trauma triggers in our past, and what COVID-19 does is it ignite those.”
We talked with Houston mental health experts about the ins and outs of trauma and how you can better understand your brain during these unprecedented times.
Trauma’s a six-letter word
We often associate the idea of trauma with those who’ve survived certain unfathomable situations, like combat veterans and victims of sexual violence, but that’s not always the case. Trauma is, in fact, much more common that you might expect.

In a nutshell, trauma is an emotional response to an event or series of events that creates a sense of fear and unpredictability, leading us to feel that our life is under threat. And life doesn’t just refer to mortality. It could also be the loss of a job, the loss of a fundamental belief, or—like in our current situation—the loss of normalcy. That “is a recipe for a lot of different traumas, meaning different sources of potential loss that people could experience,” says Christopher Fagundes, associate professor of psychology at Rice University.
Some people live through traumatic events without experiencing a change in the way they live their lives. For others, a traumatic event can fundamentally alter the way they see and respond to the world around them. “Their brain is at high alert and may perceive a threat when there is not one,” Weinstein says. “We learn from experience. If you’ve had terrible experience, you remember it, and your body remembers it.”
Why am I having a harder time coping than others?
First off, you may not be. There’s really no way to know what’s happening inside someone else’s head (we’re not mind readers). Just because your college roommate is bombarding your Facebook feed with coronavirus memes doesn’t mean they aren’t struggling too—they just might be hiding it better. “All of us for react differently to major stressors,” Weinstein says. “For one person, something can be very traumatic and another person will not experience it in the same way. It's difficult to predict.”

Still, if you’ve been having a rough go of it, it’s important to remember that just like we have different colored eyes, different hair textures, and differently shaped smiles, we also have different brains. “People's biorhythms are different,” Sarahan says. “Some people's reactions to stress are different. That’s not a fault; it’s not a failure to rise to the occasion.”
While there’s no one answer to what causes trauma, there are some ways to predict if a person will have difficulty with extreme situations. According to the experts, you may be more susceptible if:
- You’ve already experienced previous traumas, including, but not limited to, death, divorce, abuse, neglect, or bullying.
- You’re in a position of financial instability or lack a strong support system.
- You have a history of anxiety or depression, or you have a tendency to obsessively worry.
Spotting the Signs
Since we’ve established that basically everyone is feeling more tense than usual these days, you might be asking yourself, “How do I know if what I’m feeling is more than stress from the current pandemic?”
Well, we’re back to that brain thing. Since each of our brains is unique, we will likely react to trauma in different ways. Think of your family member who cries inconsolably at a funeral even though she barely knew your great aunt, versus your great aunt’s son, who goes out, gets drunk, and comes home with an earring. That being said, there are certain behaviors that crop up more frequently:
- You’re obsessing over the current situation, watching relentless amounts of news on TV, reading tons of articles, or sharing posts on social media that, whether consciously or unconsciously, stoke fears instead of providing information.
- You’re having trouble sleeping. We’re not talking about one fitful night of tossing and turning, but extreme changes from your usual sleep patterns, like you’re sleeping much more, sleeping a lot less, or are fatigued even after sleeping for hours.

- You’re isolating from friends and loved ones, avoiding video chats and repeatedly letting your cell go to voicemail, or you’ve stopped partaking in activities you usually enjoy. Sure, that’s harder to gage when you can’t lift weights at the gym or head out to Tuesday night trivia, but you might notice a lack of interest in that TV show you’ve been dying to see or that video game you’ve been marathoning.
- You’re jumping between emotions more frequently, vacillating between anger and sadness to the point of being on the verge of tears at a moment’s notice. Also, if you’re someone who has a generally sunny disposition and are suddenly looking at the world through a big, dark storm cloud, that can be a sign that something’s up, Fagundes adds. “It’s the idea that everything you’re saying comes through this lens of negativity. Not even things having to do with COVID-19, but things in general.”
Seeking Support
Let’s say you’ve noticed some of these behaviors. Now what? Most experts recommend talking to someone, whether it’s a close friend or family member. “I’ve been harping that this term ‘social distancing’ is absolutely wrong,” Sarahan says. “We need physical distance, not emotional distance.” There are also organizations, including NAMI Houston, which is part of the National Alliance of Mental Illness, that are offering online classes and support groups, as well as many mental health apps out there.
If you don’t feel comfortable talking to someone already in your life or don’t want to try a DIY approach, many therapists have transitioned to offering remote therapy. When picking a therapist, don’t necessarily focus on degrees, Fagundes recommends. “Focus on finding someone you can relate to,” he says. “The relationship you have with your therapist is the best predictor of success. If you don’t feel like that relationship is meshing with the first person you reach out to, try another one.”

Feel like you need more immediate assistance? Give the Harris Center’s COVID-19 Support Line (833-986-1919) a ring. The 24-hour help line, which has been running since March 18 and is different from Harris Center’s longstanding crisis line, offers support to those experiencing stress and anxiety related to COVID-19.
The most important thing to remember is that reaching out for help is nothing to be ashamed about. “People perceive talking about things that are hard as a weakness,” Weinstein says. “In reality, it’s easier to hold something in—stay silent about it and pretend it’s not there—than it is to acknowledge something that’s hard. That actually takes much more courage.”
If you open up, odds are you’ll find that people are feeling the same things you are. And knowing you’re not alone, especially in times of upheaval, can make all the difference.