
A Two-Centimeter Implant Could Change Your Health Forever
In 1798, Edward Jenner showed the Western world that a pinprick infected with cowpox could inoculate a child against virulent smallpox. In 1928, Alexander Fleming accidentally discovered a substance called penicillin while researching the behaviors of staphylococci. And in the last year, Alessandro Grattoni and his multicultural, multidisciplinary team of 16 researchers won approval to begin human testing on an HIV prophylactic implant so small that patients will only notice it when it’s refilled once or twice a year.
What do they all have in common? The first two men pioneered microscopic medical innovations that have since saved millions of lives. The third is on his way to joining those ranks, and it’s happening right here in Houston. But the HIV treatment is merely the innovation Grattoni and his team are furthest along in testing. His lab is currently at work developing treatments for everything from cancer to obesity.
Why is the two-centimeter-wide implant revolutionary? How many times have you forgotten to take a necessary medication? Right. The use of a nanochannel delivery system (nDS) means that will never happen again.
The device, made from a plastic called polyetheretherketone, is inserted under the skin of a person’s inner arm; inside it is a membrane that is refilled with medicine, by injection, as infrequently as once a year. It is essentially a fail-safe method for keeping a consistent flow of a drug in the patient’s bloodstream, with none of the peaks and valleys inherent in administration through pills or infusions. Doctor visits could be greatly reduced, too, since clinicians can adjust (or turn off) dosage remotely through a Bluetooth system. Essentially, drugs taken via nDS become part of the patient’s body chemistry.
How is it possible to sustain treatment for so long? That’s where drug formulation comes into play. The medication must be stable enough to last at body temperature but also diffuse with biological chemicals. A potent drug may only require a dose of one milligram to last for a significant period, slowly and steadily seeping through channels 50,000 times smaller than a human hair.

Alessandro Grattoni’s pioneering work could save countless lives. Here, he holds a wafer of membranes.
Image: Michael Paulsen
Grattoni discovered nanomedicine in Italy in 2006, when he watched fellow Italian Mauro Ferrari, one of the founders of the discipline, speak at a conference via Skype from the United States. Boiled down to its barest bones, nanomedicine, according to Ferrari, is “the notion of tiny particles that could bring drugs into the body.” Working on a nanoscale, there are no boundaries between scientific subsets like biology, chemistry or physics. Therefore, its practitioners must have some mastery of them all, a meaty prospect for a bright young scientist.
Hooked, Grattoni decided to base his master’s thesis on one of Ferrari’s theories. He presented his findings to the elder scientist after tracking him down on a train from Bergamo to Milan. Ferrari was stunned. No one else had been able to find a way to make this new type of membrane osmometer—which measures high osmotic pressure of solutions across a membrane in minutes—a device Grattoni would later patent.
It wasn't long before Ferrari invited Grattoni to join him at his then-new lab in Houston. It was a good decision: “Alessandro is a unique combination of sheer scientific talent, great executive pragmatism, and a generous commitment to making the world a better place,” he says today.
It was 11 years ago that Grattoni moved to Space City. Today, he’s chair of Houston Methodist’s department of nanomedicine, where he’s taken Ferrari’s ideas and run with them. Ferrari is now executive vice president of Houston Methodist and president and CEO of Houston Methodist Research Institute. He never imagined all the applications, from hormone therapy to HIV treatment, that Grattoni would one day be working on. “I am grandpa,” he says with a twinkle in his eye. “This is his baby.”
In his penthouse office, Ferrari pulls a large, colorful book from his well-stocked shelves. The book was a Christmas gift from Grattoni in 2015, a collection of papers both from Ferrari’s early years of nanomedical research and his later collaboration with the younger scientist, entitled, 20+ Years of nDs: The True Story of Life in Nanoconfinement. “There was no such thing as nanomedicine,” Ferrari says. “We had to invent it.”
The two men’s shared humorous streak speaks to their intelligence, of course, but may also be a testament to what’s gotten them through said nanoconfinement, a double-entendre for being trapped in the world of nanomedicine and the scientific term meaning, among other things, reduction of space for drugs to diffuse at the molecular level.
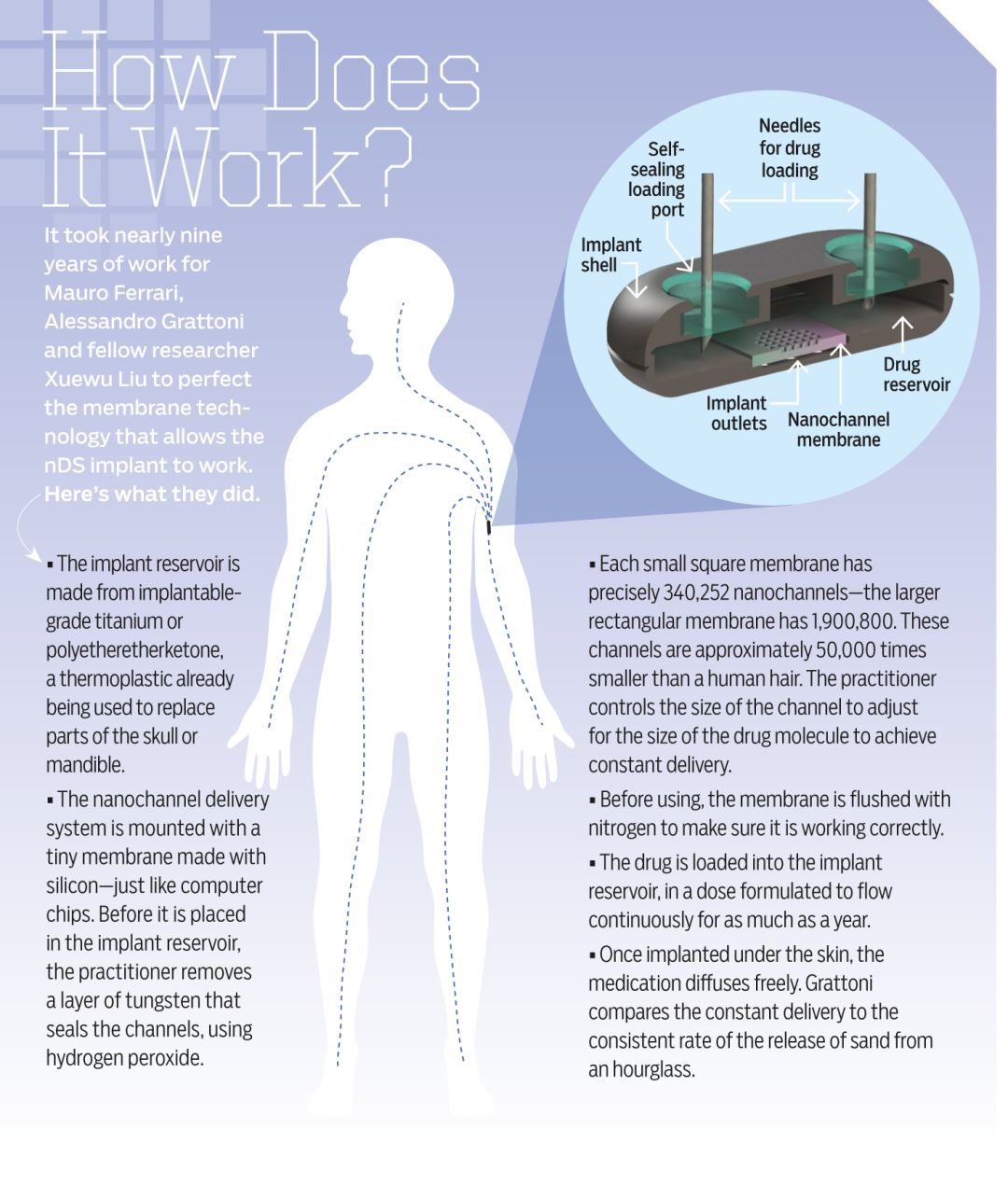
Image: Courtesy Alessandro Grattoni
The two aren’t the only scientists working on nanochannels or implants for HIV prevention. Boston company Intarcia Therapeutics received $140 million from the Bill & Melinda Gates Foundation last year for an HIV prophylactic device, an osmotic pump, which Grattoni says can be difficult and expensive to assemble.
Grattoni says his lab, too, has garnered interest from the foundation, but adds, “I cannot say that this is easy work in the sense that it’s pretty stressful. The funding is always weighing on our shoulders.” Last year, a $4 million grant from the National Institute of Allergy and Infectious Diseases helped, but far more is necessary to take the HIV project to fruition.
“If you’re too far ahead of the curve,” says Ferrari, “it’s years of loneliness.”
Today, though, with drug company Gilead Science’s participation, it appears the curve is finally rising to meet them. Trevor Hawkins, senior medical director at Gilead, believes that Grattoni’s nDS is “a game changer” that will potentially transform the way doctors deliver drugs to patients, both for chronic illnesses and prophylactically. He hopes it will be used among young women in Africa, the highest risk population for HIV infection in the world.
A company like Gilead could have chosen to work with any lab to bring their technology to the market. Why Grattoni’s? “These guys in Houston are widely published and extremely well-known in the field,” says Hawkins. “And this is a very well-designed membrane.”
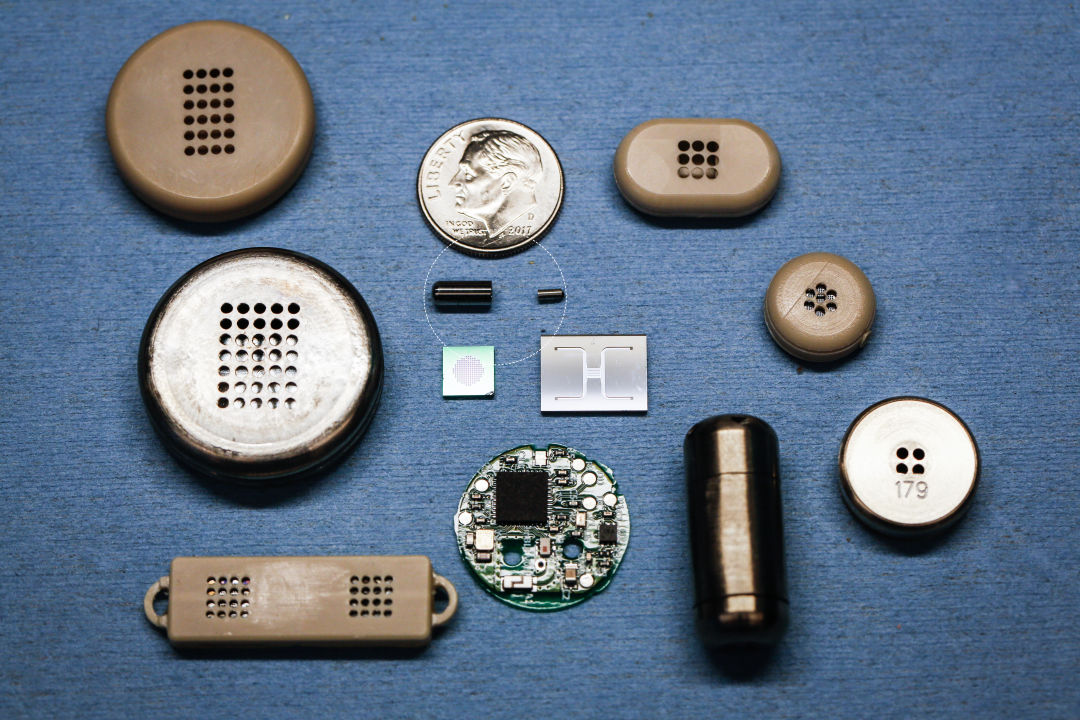
All of these devices are on their way to making big changes. The circled implant, small as a grain of rice, could fight cancer without side effects.
Image: Michael Paulsen
Within two or three years, Hawkins estimates, the nanochannel delivery system will move to human trials. At that point, Roberto Arduino of UT Health will become an important part of the puzzle, in charge of testing the prophylaxis’s safety and efficacy in treating humans. The Argentinean infectious-disease specialist was on the front lines when the AIDS crisis reared its head in the 1980s. “I used to sign one or two death certificates a day,” he recalls. He came to the United States in 1990, where matters were no better.
In those days, people infected with HIV relied on combination drug therapies that involved taking around 10 different pills two or three times a day, he remembers. Single-tablet regimens have now replaced those complex programs, with few if any side effects. But the goal is to prevent infection before it happens. Despite the wide availability of oral HIV prophylactic medications like Truvada, there are still about 40,000 new cases in the U.S. each year, “almost enough to fill the Astrodome or Reliant,” says Arduino. Cost may be a factor—a year of Truvada costs just south of $20,000 per year without insurance.
Even more troubling, other sexually transmitted diseases, including chlamydia and syphilis, are on the rise. “It means more people are having unprotected sex,” Arduino points out. And with more people putting themselves in a high-risk group, more could potentially benefit from a prophylaxis that doesn’t require taking a pill that could have catastrophic effects if it’s forgotten.
Like Hawkins, Grattoni is thinking beyond the First World. He believes his HIV implant could be even more helpful in developing countries where access to medical care is limited. If clinics in Africa, for example, were able to implant nDSes filled with an anti-HIV drug, thousands of patients could be saved. Perhaps most importantly, Grattoni thinks the method could be extremely inexpensive. To make the devices, membranes are printed out in wafers of 700 and then placed in their polyetheretherketone cases—something that, all told, potentially costs less than the drugs contained therein.
Gilead, which was central in developing single-tablet HIV regimens, is on board to help create a medication that will release slowly and steadily through the nDS implant. Once inserted, a single tablet of that drug could last six months, a year, or possibly more, says Grattoni.
Before Gilead came on board this spring, animal testing was a necessary part of the process. Trials began close to a decade ago with testing on rats, before moving on to pigs and non-human primates. Immunologist Jagannadha Sastry, a researcher and professor at both UT Health and MD Anderson, was in charge of the animal trials for the HIV project. His four-year study was the final piece of preliminary data necessary to prove that the treatment would work.
And while the HIV prophylaxis is the closest to being available to human patients, many other applications of this new technology are already well into their animal-testing phases. One of the most promising could make obsolete the whole-body toxicity that is chemotherapy, which often comes close to devastating patients as much as cancer itself. The most progress thus far has been made in attacking breast cancer, but Grattoni believes the nano treatment could defeat “so many cancers.”
He and his team have successfully completed rodent testing on a half-centimeter implant that can be injected into a tumor, releasing an immunotherapeutic drug that they believe would not only kill that cancer, but also create what’s known as an abscopal effect. Essentially, combined with radiation, the localized treatment activates an adaptive immune response that also makes war on metastases elsewhere in the body, including tumors that doctors haven’t yet identified in the patient.
“Potentially, this can have zero side effects,” Grattoni says. “They’ve already shown in some instances that it’s like a miracle in the patient. Treating cancer with zero side effects—it would be quite phenomenal.”
Image: Courtesy Alessandro Grattoni
T
he walls of Grattoni’s office are bedecked in whiteboards dense with jottings that look almost like an alien language to an outsider. Perhaps it’s appropriate, then, that one of the few personal touches is a sticker from NASA, the kind that might be plastered on a Trapper Keeper. That’s because Grattoni’s research may have applications beyond planet Earth.
Another of the scientist’s many titles at Methodist is director of space nanomedicine. Four of his projects have been approved for testing that will take place without the bonds of gravity. This is thanks to grants from the Center for the Advancement of Science in Space, a nonprofit that funds research on NASA’s International Space Station.
One experiment has already blasted off. The next, in conjunction with drug company Novartis, will launch in November. This experiment, performed by astronauts trained to follow procedures just as members of Grattoni's lab would on terra firma, will observe the treatment of muscle atrophy in rats. This makes sense, because while a large portion of atrophy sufferers are elderly patients confined to bed, astronauts also lose muscle and bone during long flights. Rodents do, too, but steady doses of medication could make that a thing of the past.
Drug testing is a long haul, and proving the safety and efficacy of an entirely new way of administering medications even more arduous. But to Grattoni, the 11 years that have passed since his arrival in Houston mean little compared to the tiny everyday miracles that will soon take place in patients’ lives. In the United States and Africa alike, one of the world’s most fearsome killers is about to meet a minute new enemy. Human immunodeficiency virus won’t know what hit it.













































